What is the role of the ophthalmologist in increasing therapeutic compliance?

João Filipe, MD
Introduction
Therapeutic compliance or adherence refers to all the aspects that characterize the cooperation of the patient with the medical indications by following a correct administration of the prescribed therapy.1 Compliance is fundamental, because null adherence equals null treatment and progression of the glaucomatous damage.
We can divide the concept of compliancei into:2
· Fulfillment - correct execution of the prescribed therapy: route and mode of administration, time and dose (note: compliance may have fulfillment as a strict meaning; we will use the broad meaning of compliance).
· Persistence - fulfillment of the prescribed treatment is adequately maintained, i.e. it is the length of time the patient respects the medication until he/she discontinues it.
• Example: 1: The patient prescribed with prostaglandin who takes the medication for only 6 months, suspending it without medical indication, failed to persist.
• Example 2: The patient medicated with a fixed association to be applied every 12h but who takes it only at night, and who buys the fixed association eye drops every month, has a correct persistence, despite having a 50% fulfillment.
Another concept is the “white coat adherence”,1 in which the patient’s compliance increases noticeably a week before the clinical visit and decreases again after it.
We describe methods of estimating the compliance in patients with glaucoma and, consequently, methods to improve it as an integral part of glaucoma treatment.
Scientific evidence
Although the therapeutic efficacy of the drugs for glaucoma is clearly demonstrated, the lack of compliance presents itself as a public health problem.3 Several studies have identified an association between non-compliance and increase in the rate of visual loss,4 worse therapeutic results and even increase in healthcare costs.5 It is also suggested that persistence is usually 33-39% over a year of initial glaucoma treatment.2 Adherence to therapy and persistence in patients with glaucoma is lower than the one documented for other chronic diseases (diabetes, dyslipidemia, osteoporosis).6
Compliance is an intuitive concept, but the lack of compliance in a patient can be difficult to detect for several reasons:2,7
· The patient wants to be “accepted” and to please the doctor, so they will not easily admit that they are not complying with what we prescribed
· The patient doesn’t want to be judged
· Non-adherence is a socially undesirable behavior
· The patient wants us to think he/she is a “good patient”
· It is difficult to measure accurately the patient’s compliance
A systematic review assessed objective compliance measurement studies7 and concluded that persistence is low (at 12 months of treatment it is 67%, ranging from 62% to 78%), as well as fulfillment (56%, ranging from 37% to 92%). There are several methods of measuring compliance that we can and should use (Table 1).
|
Table 1. Examples of methods to measure compliance.7 |
According to the study GAPS8 - Glaucoma Adherence and Persistence Study - ophthalmologists consider that between 20% and 33% of patients do not obtain benefits from the medication due to lack of adherence, and they detect between 25% and 33% of patients with lack of compliance. The rate of non-adherence to therapy is estimated to be between 30% and 70%, but patients overestimate their therapy fulfillment and persistence rate.1
· Poor compliance risk factors:
There are several factors associated with low compliance,2,9,10 which the ophthalmologist must identify and correct (Figure 1). A recent review study9 identified in the current bibliography the eleven main causes of non-compliance:
1. Skepticism on the efficacy of the medicine
2. Skepticism that glaucoma causes vision loss
3. Poor level of information on the disease
a. 14% of the patients2 do not know that they may lose their vision because they do not put in eye drops
4. Low personal efficacy
5. Forgetting
a. lack of routines and strategies to help remember the moment at which drops should be applied
b. multi-pathology: administration of several medications daily leads to forgetting and administration errors
6. Cost
a. 25% of the patients referred as reason for lack of adherence the cost of hypotensive medication (even if it is small)2 that has been increasing in Portugal
7. Difficulties associated with the application of the eye drops
a. presence of another physical pathology that makes it difficult to apply eye drops - discompliance1
8. Difficulties associated with respecting the application schedule
a. 15% of the patients reported difficulties in complying with the therapy when traveling2
9. Side effects
10. Lack of confidence in the doctor
11. Stress
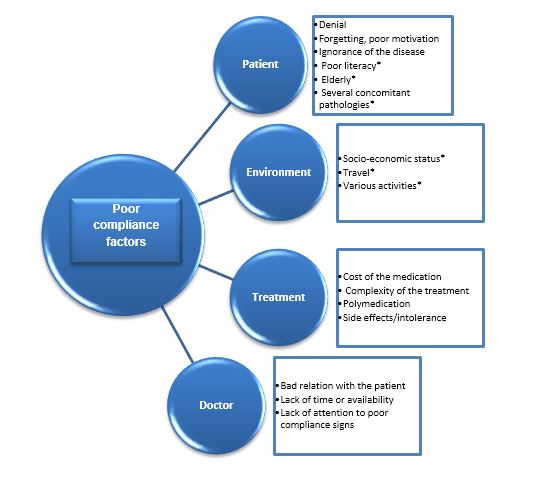
Fig.1 Some factors frequently responsible for the patient’s poor compliance
Poor compliance may include several different attitudes from the patients:
· Lack of administration of the prescribed medication
· Excessive use of medication or administration of non-prescribed medication
· Interval span between administrations or inaccurate posology
· Use of the therapeutics for the wrong objective
· Side effects
In addition, glaucoma is a chronic pathology5, asymptomatic until late stages, another factor that impairs compliance (we often use the aphorism “one doesn't feel the glaucoma, one feels the therapy” when referring to the discomfort or adverse effects which therapy can cause to the patient, thereby reducing adherence). The temptation not to comply is great because the patient does not feel the initial progression of glaucoma, but often feels discomfort when applying the eye drops prescribed.
· Measures promoting compliance:
It is up to the ophthalmologist to prescribe the appropriate therapy when confronted with the diagnosis of glaucoma, but also and not least, to make sure that his/her patient follows the therapy. The first step in combating lack of compliance is its identification. In addition to modifying the low adherence factors, therapeutic adherence can be enhanced with multifaceted measures based on:3,10,11
1. Education:3
a. raising the awareness about the pathology, its progression and the importance of the treatment
b. holding the patient responsible for the therapeutic action plan
c. videos showing how to put the eye drops and application training
d. positive reinforcement in cases of good adherence
2. Therapeutic customization:3
a. adjustment of the therapeutic schemes to routines and the patient’s physical capacity
b. alert systems (mobile applications)
c. alliance1 - involve a family member/caregiver to respect the correct therapy
3. Simplification:
a. use fixed associations
b. write the posology and the instructions in an objective way:
Example:
DO NOT write: 2 x day
Write: each 12 hours
c. avoid/reduce side effects
d. eye drops in a visible place
4. Compliance check in all consultations:
a. open questions,10 focused on the patient, thus making it easier to detect non-compliance
Adequate question: “What difficulties did you have to apply the drops?”; “How many times did you forget to apply them this week?” Patient understands that they can express their shortcomings, allowing the doctor to implement measures to improve compliance.
Inappropriate question: “You did apply the medication correctly, right?” Patient with no room to admit non-compliance.
b. question whether the medication prescribed at the last visit was enough
We should insist and persist, without ever giving up on this arduous and relentless task of encouraging continuous compliance, with the ultimate goal of maintaining the patient’s vision and quality of life1 for as long as possible.
