What is the role of the biodegradable collagen matrix implant (Ologen) in trabeculectomy?

Maria da Luz Freitas, MD, FEBOS Glaucoma
Introduction
Ab externo trabeculectomy is a bleb-dependent filtering surgery, the success of which relies on the modulation of the scarring process.1
The failure associated with the healing process is the result of an inflammatory process, fibroblast proliferation and extracellular matrix synthesis.2
The different components of this process are triggered by the surgery itself, but are often already present before the surgery.
They are caused or potentiated by iatrogenic factors, such as chronic use of topical therapy, with or without associated allergic component, presence of previous surgeries, uveitis or neovascular secondary glaucoma, or even associated with constitutional factors, such as race and young age.
There are no well-established protocols guiding the best strategy to reduce the possibility of surgical failure due to wound healing processes and, consequently, increase the filtration rate and survival. It is difficult to conduct meta-analyses in this surgical field given the lack of randomized studies with similar populations, same surgical techniques, same surgeons, same follow-up periods and same criteria and methods of evaluation. There are, however, a number of recommendations in which the best strategy is left to the discretion of the surgeon, having in mind the particular patient. Some examples are the substitution of the topical therapy (essentially prostaglandin analogues, prostamines and brimonidine) by systemic therapy one month prior to surgery and the use of fluorometholone or topical non-steroidal anti-inflammatory drugs 15 to 30 days before surgery.3,4
As intraoperative strategies there are a number of possibilities, often resulting from personal experience or beliefs, and others are well studied in terms of benefit and surgical risks: low cauterization, tenectomy, use of antimetabolites (5-Fluorouracil and Mitomycin C), shapers, also called creators of space (matrix of biodegradable collagen-Ologen®), use of anti-VEGFs, injection of subconjunctival corticosteroids at the end of surgery. As postoperative strategies there are multiple periods of use and types of steroidal and non-steroidal anti-inflammatories to choose from.1 There is also the possibility of using antimetabolites and needling associated with different medicines (for example: antimetabolites, anti-VEGFs).
In spite of their off-label use, the advance that the antimetabolites brought in the 1980s to the control of the bleb filtration healing process in a multitude of clinical situations is impressive. As we all know, 5-Fluorouracil (5-FU) acts selectively on the S phase of the cell cycle, inhibits fibroblast growth, reduces the type I collagen, fibronectin and cell migration for one week after its use. Initially, a 0.1 ml of 50 mg/ml injection was administered in the postoperative period, adjacent to the bleb, and sometimes more than once, which resulted in an increase in the number of control visits and discomfort to patients. In recent years, its use was extended to the surgery itself, soaked in a sponge or pressed cotton, in a concentration of 25 or 50 mg/ml up to 5 minutes.
Mitomycin C (MMC), 100 times more potent than 5-FU, has a longer effect (about 1 month). It inhibits the DNA replication, mitosis, RNA and protein synthesis and thus inhibits the growth and proliferation of fibroblasts and endothelial cells present in the healing process. Initially its use was exclusively intraoperative. Exposure concentrations and times have never been well established: the concentration used may range from 0.1 to 0.5 mg/ml and the exposure time may vary from 1 to 5 minutes. More recently, it also came to be used in the postoperative period, adjacent to the filtration bleb, in the form of an injection of 0.1 ml at a concentration of 0.02 mg/ml. Like all active substances, it has effects considered to be secondary to the intended primary effect. Some of the side effects are specific to each active principle, but others are common to both products, such as an increased risk of severe hypotonia, persistent outward drainage of the bleb (bleb leakage) and increased localized bleb infections (blebitis) or even endophthalmitis. Stamper et al.5 describe that hypotony maculopathy with the use of 5-FU is more frequent and accentuated at young age and moderate myopia, and Whiteside-Michel J et al.6 estimate it happens in 5% of the cases when used at a young age. According to Smith MF et al.7, bleb leak with intraoperative 5-FU (50mg/ml) appears in 8% of the cases after 1 year of follow-up. The incidence of filtration bleb infections ranges from 1.9 to 13%, versus the 0.2 to 4.8% risk in the case of simple trabeculectomies, at the same follow-up interval.8 5-FU has other particularities, such as potentiating ocular surface defects, including punctate keratitis, and epithelial defects that are sometimes difficult to resolve. The use of MMC can cause hypotony maculopathy in about 8.9% of the cases9. According to WunDunn et al., bleb leak with intraoperative use of 0.2mg/ml for 2 minutes after 1 year of follow-up is 6.8% 10. The incidence of filtration bleb infections with MMC with follow-up periods between 16 months and 8 years varies between 1.5% and 13.8%.8 Greenfield et al.11 found that the incidence of blebitis at 16 months of follow-up was 2.1% with MMC versus 0.2 to 1.5% when no antimetabolites were used. Other important side effects related to MMC are corneal endothelium irreversible damage upon accidental entry of MMC into the anterior chamber and toxicity to the ciliary body if there is direct contact. However, the greatest criticism of MMC is the possibility of creating thin and avascular filtration blebs, often large in size, which increases the risk over the years of rupture, infection and permanent discomfort with changes in the ocular surface (Fig. 1).
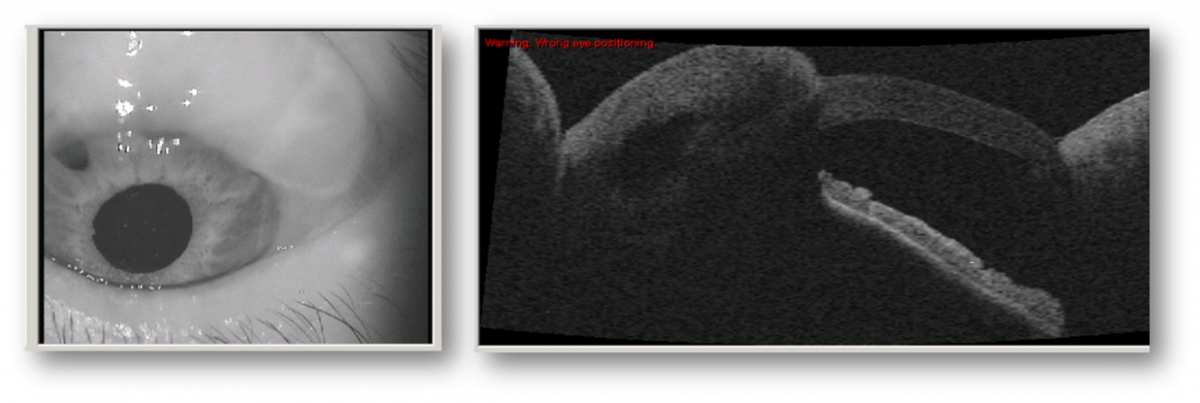
Fig. 1 – Mitomycinic filtration bleb
A comparative case-control type study carried out by Jampel, with the objective of determining the risk factors for late infection of filtration blebs, found that the isolated use of MMC conferred a relative risk of 2.45.12 In a retrospective review of endophthalmitis related to filtration blebs, Song et al.13 found that 82% of the infected eyes (40 out of 49 eyes) in the same institution and over a period of 15 years involved the use of antimetabolites (33 eyes operated with MMC and 7 eyes operated with 5-FU).
What is the biodegradable collagen matrix implant?
At the beginning of this century a new biodegradable collagen implant emerged – the Ologen®. Ologen® is a flexible biodegradable collagen matrix of animal origin whose porous matrix structure (0 – 300 μm) is obtained by cross-linked lyophilized type I atelocollagen (> 90%) and glucoseaminoglycans (<10%). Due to having good immunological tolerance, it began to be used as a shaper or creator of space in filtering surgery, replacing the antimetabolites or in combination with antimetabolites in low doses. It is an absorbent implant, which does not increase the volume or pressure on the surrounding structures, but optimizes and stabilizes the injured area in order to model the connective and epithelial healing processes. Its mechanisms of action are described as the ability to maintain a barrier between the filtration bleb and the subconjunctival tissue, preventing cell migration and fibroblast formation through its porous formation as well as the ability to absorb the aqueous humor and prevent tissue contraction. A history of hypersensitivity to porcine collagen is a contraindication and, as with antimetabolites, no safety studies were conducted in children and pregnant women. A possible advantage over the use of antimetabolites is the fact that the filtration blebs obtained are flat, with no increased risk of hypotonia, infection or bleb leak. If there are signs of allergy or presence of hypotony maculopathy, it can be removed. It also seems to reduce the need for needling or antimetabolite injections in the postoperative period.
There are several models, but the ones most used in ab externo trabeculectomy are those with a 6 mm diameter and 2 mm thickness and those with a 12 mm diameter and 1 mm thickness. They can be used in whole or sectioned (Fig. 1), according to the clinical situation.
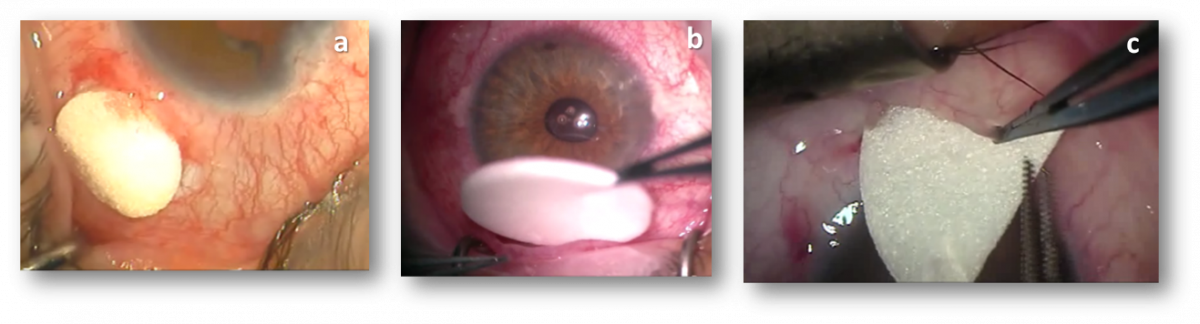
Fig. 2- a. 6 mm x 2 mm implant; b. 12 mm x 1 mm implant; c. implant sector
Indications of the biodegradable collagen matrix implant
The indications for the use of the Ologen® implant alone or in combination with MMC at low dose in ab externo trabeculectomy are the same as for the use of antimetabolites: failure of previous filtering surgeries, congenital or juvenile glaucoma, primary glaucoma in young adults, black race, secondary glaucoma (uveitis, neovascular), conjunctival fibrosis due to chronic use of eye drops, previous eye surgery.
The surgical technique, removal of the implant and different clinical cases are presented in a separate text: Use of the biodegradable collagen matrix implant in trabeculectomy – surgical technique and clinical cases.
Publications
The lack of randomized or non-randomized studies or case-control studies with similar populations, in terms of age, type of glaucoma, severity, type and duration of eye drops use, with the same surgical techniques, same surgeons, same follow-up periods and same criteria and methods of evaluation, lead to the difficulty of performing consistent meta-analyses and comparative evaluations in this surgical field.
Similarly to what has already been described for the side effects of antimetabolites’ use, we found a discrepancy in the results of the studies and comparative analyses of patients operated with Ologen® versus antimetabolites or simple trabeculectomy with respect to efficacy and safety.
Despite this reality, I cannot fail to mention and comment on some publications.
Cilino et al.14 published in 2016 a comparative, randomized study with a follow-up of 5 years of 40 eyes submitted to trabeculectomy with Ologen® or MMC. At the end of the 5 years follow-up, the Ologen group showed equal efficacy and an equal or even higher safety. The concentration of MMC used was 0.2mg/ml during 2 minutes and 6x2mm collagen implant. In the postoperative period, 0.1% dexamethasone was used for two months. Primary open-angle glaucoma and exfoliative glaucoma were included in the study, with eyes with previous surgeries or history of trauma being excluded.
In another study15, prospective, randomized and with a follow-up of 5 years, an Ologen® implant (7mmx4mm) was placed in 31 eyes and MMC (0.2mg/ml during 2 minutes) was used in 32 eyes. In the postoperative period, 0.1% dexamethasone was used for 6 weeks.
In this study, Ologen® showed a complete success rate, qualified as higher than that of MMC, as well as different size and vascularization of the blebs in both groups. The postoperative complications in the two groups of studies did not differ.
The study conducted at the Zhongshan Ophthalmological Center16 concluded that the Ologen® implant and MMC in trabeculectomy have the same efficacy in the reduction of intraocular pressure, reduction of the number of medications, success rates and tolerance. However, they advise caution in interpreting the results because the clinical relevance is still limited.
In 2015, Q Ji and colleagues compared the efficacy and safety of the Ologen® implant with the use of MMC. The article refers an equal long-term success rate with the implant, but there seems to be no advantage in avoiding the complications related to MMC.17
What is then the relevance of the biodegradable collagen matrix implant in trabeculectomy?
Implants seem to be a safe and effective alternative to the use of antimetabolites in ab externo trabeculectomy. Their efficacy seems to be at least similar to that of MMC, with the advantage of being removed in case of hypotonia. The filtration blebs are flat, vascularized without increased risk of hypotonia, infection or bleb leak.
