How to make the transition from conventional trabeculectomy to the modified Moorfields Safer Surgery trabeculectomy?

Fernando Trancoso Vaz, MD
The trabeculectomy described in 1968 by Cairns1,2 (Conv Trab) differs very little from that performed today. The procedure consists in the creation of a protected fistula from the anterior chamber (AC) to the subconjunctival/subtenonian space. Despite its efficacy, it is associated with a relatively high complication rate due to excessive drainage of aqueous humor: hypotonia, athalamia, choroidal detachment, hypotony maculopathy and suprachoroidal hemorrhage3. The technique of the modified Moorfields Safer Surgery System trabeculectomy (MSS Trab), developed by Peng Khaw and colleagues in 2005, reduces these risks and ensures greater safety4-6.
We started using this modified technique in our service at the end of 2008. The main differences introduced are:
. Performing a fornix-based conjunctival incision with an extensive subconjunctival dissection. We went from the Conv Trab limbus-based conjunctival incision (incision at 7 mm from the limbus) to a fornix-based incision (incision at the limbus level, 1 mm from it, making a limbal peritomy with a 6-8 mm extension) (Fig. 1) in MSS Trab. On the other hand, while in Conv Trab only the region near the flap is submitted to debridement, in MSS Trab a wide and posterior dissection is made towards the fornix (10-15 mm), in order to create a large filtration area and to avoid delayed complications of the bleb, such as leakage or Bleb cyst entrapment (Fig. 2).
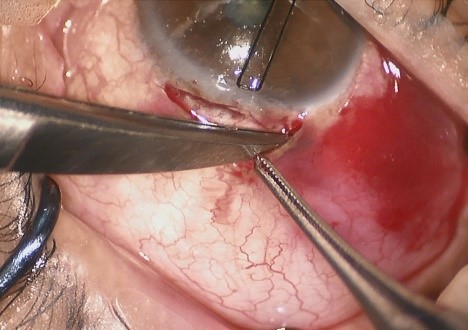
Figure 1- Fornix-based conjunctival incision (peritomy)
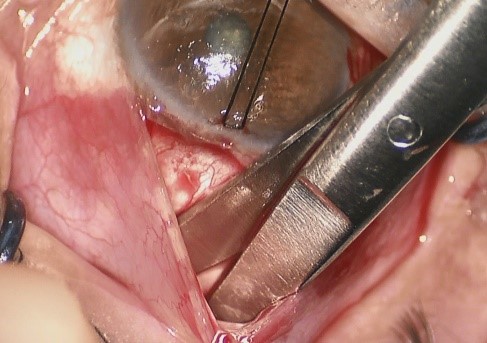
Figure 2- Wide and posterior conjunctiva/Tenon dissection
· Creation of a scleral flap that is 0.5-1 mm from the limbus. Unlike the Conv Trab in which the scleral flap goes up to the limbus, in MSS Trab, the 4x4 mm quadrangular flap is delimited with a 15° blade, and then dissected with a disc blade up to a 0.5-1mm distance of the limbus (Fig. 3). From this point, the dissection is made only in the central region (Fig. 4), in order to stimulate the posterior drainage of the AH and the creation of a more diffuse and non-cystic bleb, also avoiding its lateral extension near the limbus.
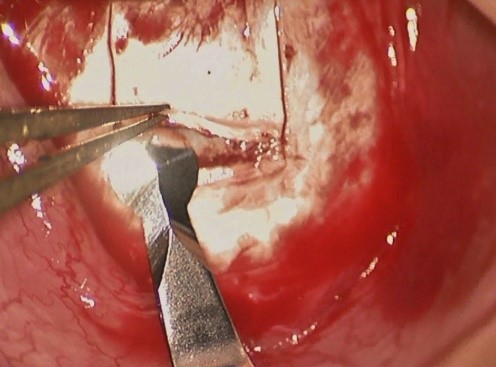
Figure 3- Scleral flap (dissection with disc blade)
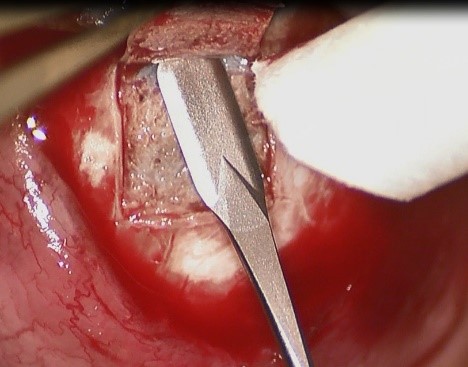
Figure 4 - Scleral flap (dissection in the central region near the limbus)
· Application of antifibrotics in a wide area. The choice of antifibrotic, if necessary, should be stratified according to the risk factors for surgical failure. We use the Moorfields/Florida “More Flow” classification: MMC 0.2 mg/ml intermediate risk and MMC 0.4 mg/ml high risk7. The application is made with polyvinyl alcohol sponges (less risk of fragmentation, thus lower risk of fragments of intraoperative material), ideally for 3 minutes (experimental pharmacokinetic studies on the inhibition of fibroblasts with MMC showed that inhibition of all fibroblasts was observed after 3 minutes of exposure, with a plateau inhibition being reached, the antifibrotic effect achieved beyond this period being very slight, and that between 1-3 minutes the inhibition is exponential and less predictable with considerable variation in the dose of drug delivered and thus in its antifibrotic effect7), in the previously dissected area as well as under the scleral flap (Fig. 5). The edges of the conjunctiva should not touch the sponges. A thorough washing with saline follows.
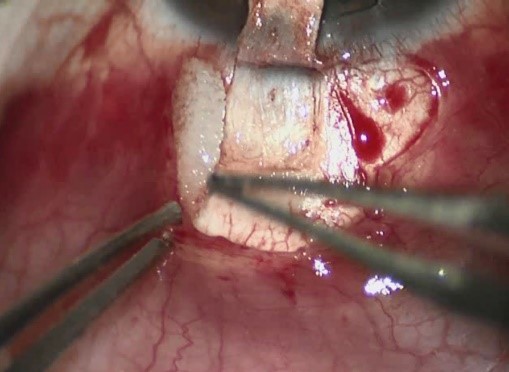
Figure 5 - MMC application
· Use of an AC Maintainer during surgery (serum continuous infusion). After making two sutures at the vertices of the flap (without squeezing, just so that they stay in place – “pre-placed sutures”), a paracentesis is made parallel to the limbus (Fig.6), with a long intracorneal path length (we use a Clear Cut blade – 1mm from Alcon), followed by an infusion line (we use a Lewick 20G stabilizer – Katena K20-3271), attached to a BSS bottle at 30 cm from the eyeball (1 drop/3-4 seconds, causes IOP 10-15 mm Hg)8.
Figure 6 - Placement of an AC stabilizer
· Performing a standardized sclerostomy with punch. Removal of the sclera at the Conv Trab is done with a 15º blade/Vannas scissors, and the size of the sclerostomy can vary greatly. In MSS Trab, after entering the AC with a 15º blade, the sclerostomy is done using a 0.5 mm punch (Khaw Small Descemet Membrane Punch No. 7-101 - Duckworth and Kent) placed vertically to create a non-valved sclerectomy (Fig.7).
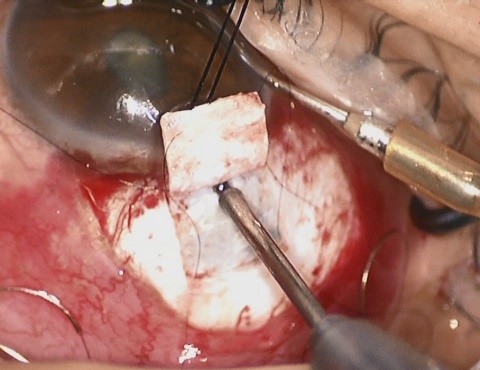
Figure 7 - Sclerostomy with punch
· Iridectomy broad at the base and short in length.
· Use of additional so-called adjustable/removable scleral sutures. In MSS Trab, and unlike Conv Trab, in addition to the two fixed sutures, two more adjustable/removable sutures are made on both sides of the flap according to the path represented (Fig. 8). It begins in the sclera parallel to the flap (step 1), followed by a transscleral/transcorneal path (non-transfixive), it comes out of the cornea and re-enters the cornea a little to the side (step 2), following again a transcorneal path and, after that, below the flap, up to half the flap near the lateral border. It re-enters the sclera, a little bit ahead, creating a loop (step 3), crosses the thickness of the flap and enters the adjacent sclera leaving it a few mm from the side of the lateral border (step 4). Make four loops and tighten. The degree of tightness is determined by the amount of AH that passes below the flap (ideal - slight ooze) using a micro sponge (Fig.9 - VIDEO).
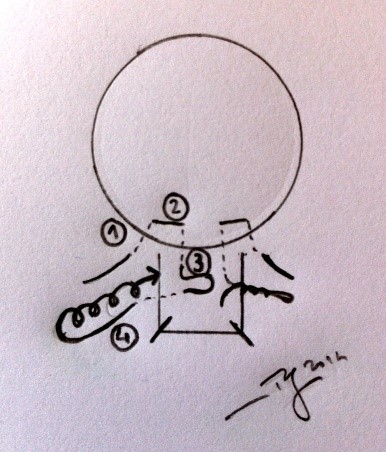
Figure 8 - Schematic of the adjustable sutures
Figure 9 - Adjustable suture
The advantage of these sutures is that they can be adjusted/removed postoperatively if IOP is higher than 15mmHg.9,10 The adjustment can be done under local anesthesia, at a slit lamp and with forceps with smooth edges, pressing the knot and making small lateral movements of 1mm, or towards the cornea. Alternatively, the suture may be cut on its way into the cornea, and simply pulled and removed. If MMC is used, this step should not be done before the fir1st postoperative month. Adjustment/removal of the suture is effective only while there is no major scarring (first 3 weeks) and can be extended up to 8 weeks if MMC is used.11–13
· Conjunctival closure. There are several ways to close the conjunctiva: 2 stitches at the ends of the conjunctival incision14 (sometimes complemented by a mid-distance “paranoia” suture10), continuous suture near the limbus, or stitches anchored in corneal grooves. Since the authors tried different closure modalities and did not notice differences in terms of leak tightness, we opted for the first solution because it was the least time-consuming.
Concluding ... How to move from Conv Trab to MSS Trab?
The main steps to be taken for this transition are a fornix-based conjunctival incision with an extensive subconjunctival dissection, creation of a scleral flap that is 0.5-1 mm from the limbus, application of antifibrotics in a wide area, use of an AC Maintainer during surgery (continuous infusion of saline), performance of a standard sclerostomy with punch, iridectomy with a broad and short length, use of additional adjustable/removable scleral sutures, and conjunctival closure with 2 stitches at the ends of the conjunctival incision.
All these small changes introduced with MSS Trab are easy to apply, quick to learn and allow greater reproducibility in the technique, thus ensuring greater safety and control of the intraocular pressure, with fewer postoperative complications and without using expensive materials or devices.
