What is the role of antimetabolites as intra- and postoperative adjuvants?

Fernando Trancoso Vaz, MD
In trabeculectomy, a communication – protected sclerectomy – is created to drain the aqueous humor into the subconjuntival space, resulting in a filtration bleb. During the normal healing process in the postoperative period, the development of fibrosis at the episcleral-conjunctival interface is one of the main causes of surgery failure. To modulate wound healing, several pharmacological agents can be used as intra- and/or postoperative adjuvants. Despite a recent interest in new molecules, 5-fluouracil (5-FU) and mitomycin C (MMC) are still the most widely used drugs for this purpose.
5-FU acts by antagonizing pyrimidine metabolism, inhibiting DNA replication and suppressing fibroblast activity. MMC is a non-specific alkylating agent whose active metabolite will cross-link with DNA molecules, thereby inhibiting DNA synthesis. Unlike 5-FU, MMC acts not only on fibroblasts, but also on endothelial cells, being 100 times more potent than 5-FU and inhibiting fibroblasts for 30 days (vs. 1 week with 5-FU).
The dose, the exposure time and the application area will influence the outcomes in terms of antifibrotic effect. There is some variability in the antimetabolite dose, duration and area of exposure. For intraoperative use, the European Glaucoma Society (EGS) recommends either 25-50 mg/ml 5-FU for 5 minutes, or 0.1-0.5 mg/ml for 1-5 minutes MMC, administered with a sponge. In the postoperative period, injecting 0.1 ml of 5-FU 50 mg/ml or MMC 0.02 mg/ml is recommended. It should be highlighted that although 5-FU is mentioned in EGS Guidelines, it is becoming less used intraoperatively, and it is now most used in the post-operative period, either or not associated with needling. In vitro studies (1990 and 1993), suggest that fibroblast inhibition by MMC only depends on concentration and not on time, indicating that MMC sponge application for either 1- or 5 minutes would have the same efficacy. A clinical study by Zacharia PT et al. (1993) shows that tissues would be saturated with MMC after a 1-minute application. According to studies by Manners T et al. (2001), IOP control was the same using MMC for either 2 or 5 minutes.
In vitro pharmacokinetic studies with MMC (1993 and 2004) showed that after a 3-minute exposure all fibroblasts were inhibited. Subsequently, inhibition reaches a plateau, with little effect observed beyond 3 minutes. Between 1 and 3 minutes, there is considerable variation in the dose of captured drug, and hence on the degree of fibroblast inhibition. Consequently, the authors recommend a 3-minute application time, and varying the antifibrotic effect with the MMC dose, which would be applied diffusely in a large area so as to obtain a diffuse bleb. This is the standard procedure in our department.
Peng T. Khaw et al. suggest that the choice of agent and duration of exposure be stratified according to risk factors for fibrosis and complications. Patients are therefore classified as low, intermediate, or high risk for glaucoma surgery failure, according to the Classification Risk Moorfields Eye Hospital/University of Florida Risk Classification (Tab.1). In low risk patients, either no treatment or 5- FU 50 mg/ml for 5 minutes can be used; in moderate risk patients, 5-FU 50 mg/ ml for 5 minutes or MMC 0.2 mg/ml for 3 minutes; in high risk patients, 0.5 mg/ ml MMC for 3 minutes is used.
Antimetabolites in the postoperative period should be applied around the filtration bleb, with or without associated needling (Fig. 1), in patients showing signs of scarring and imminent risk of bleb failure (increased vascularity, thicker and less mobile conjunctiva, smaller and flatter bleb, "corkscrew" vessels), even with normal IOP. As a rule, the functionality of at-risk blebs should be restored whenever possible (using corticosteroids, 5-FU, etc.) before proceeding to further surgical procedure.
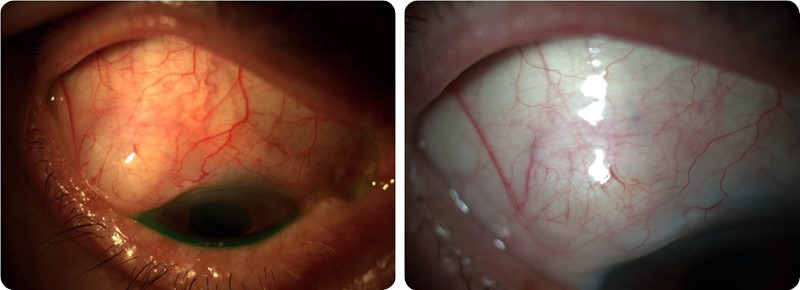
Fig.1 Needling with 5-FU - Apperance before (A) and after (B) needling (diffuse and less vascularized bleb).
In spite of the advantages of reducing surgical failure rate, the use of antimetabolites can also cause an increase in postoperative complications (leakage, hypotonia, choroidal detachment, and infections – blebitis or endophthalmitis). The Moorfields Safer Surgery (MSS) modified trabeculectomy aims to reduce some of these bleb-related complications by making a fornix- based conjunctival incision and applying antimetabolites in a more extensive area, thus avoiding cystic and localized blebs (Fig. 2).
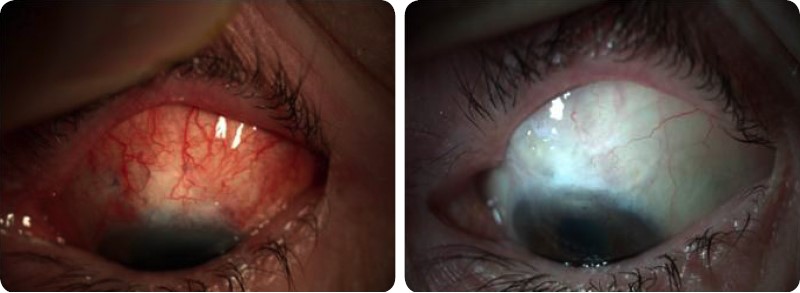
Fig.2 Moorfields Safer Surgery (MSS) modified trabeculectomy – MMC diffuse application – Bleb appearance 1 day (A) and 1 year after surgery (B).
Among other recently studied agents for the modulation of postoperative scarring, antiangiogenic factors (anti-VEGFs) such as bevacizumab (Avastin®), and physical barriers such as OloGen® can be highlighed. However, there is still insufficient evidence that they may replace MMC. Besides antiangiogenic properties, bevacizumab has been shown to have anti-inflammatory and anti- fibrotic properties,, with a decrease in polymorphonucleated cell migration and fibroblast proliferation, thus inhibiting collagen deposition. It persists longer in tissues by becoming attached to the sclera. OloGen® consists of a porous matrix of collagen-glycosaminoglycans, reorientating the deposition of collagen fibers along their bundles and preventing healing compacting, thus aiming to reduce the need of antimetabolites5. It is degraded after 90-180 days.
