The Role of Anterior Segment Imaging in II. Glaucoma Surgery Outcomes Assessment

Helena Filipe, MD, MSc
Summary
This paper aims to appraise the role of anterior segment imaging in the surgical management of glaucoma. The illustrative imagiograms were acquired utilizing both technologies. We describe information interpreted upon anterior segment imaging that can be relevant to assess glaucoma surgery outcomes and hence the best clinical follow-up.
Introduction
The filtering bleb aspects found at the slit lamp may not always correspond to the expected intraocular pressure surgery outcome. Bleb features found in UBM and AS-OCT cross sectional images can help in the investigation and provide clues on the reasons behind those results to guide the best management strategy.1 We will explain the main imaging characteristics associated with functional filtering blebs and its correlation with aspects found in the confocal microscopy; how anterior segment imaging demonstrates the efficacy of laser procedures onto the iris; the importance of these technologies in the pre and post operative care in glaucoma surgery using anterior with posterior drainage devices; the aspects related to minimal invasive glaucoma surgery and the clinical application in cycloplastia.
Filtering Glaucoma surgery
UBM and AS-OCT substantially complement optical biomicroscopy in filtering glaucoma surgery post-operative assessment. Yamamoto has proposed a system of classification correlating the filtering bleb’s ultrasound characteristics and the surgery success. The internal echostructure of the filtering bleb and the presence of an intrascleral route have shown good correlation with intraocular pressure control (type L bleb).2 Table 1
Based on AS-OCT morphology and internal reflectivity, Labbé and associates defined four types of filtering blebs: diffuse, microcystic, flattened and encapsulated. Good intraocular pressure control was associated with diffuse and microcystic filtering blebs (Fig 1).3,4 Table 2
Table 1. Filtering bleb ultrasound characteristics according to Yamamoto. Type L blebs showed the best intraocular pressure control immediately followed by type H blebs.
|
UBM |
Low reflectivity |
High reflectivity |
Encapsulated |
Flat |
|---|---|---|---|---|
|
Internal reflectivity |
Reduced-moderate |
High |
High |
High |
|
Subscleral route |
Visible |
Usually visible |
Visible Visible |
Absent |
|
Cystic spaces with fluid |
Possible |
Possible |
Cavernous |
Absent |
|
Height |
Moderate-high |
Variable |
Variable |
Flattened |
Table 2. Characteristics of the filtering bleb according to Labbé et al. based on AS-OCT imaging and correlation with in vivo confocal microscopy. Diffuse and cystic blebs showed the best intraocular pressure control
|
AS-OCT |
Diffuse |
Cystic |
Encapsulated |
Flattened |
|---|---|---|---|---|
|
Suprascleral reflectivity
|
Reduced
|
Reduced
|
High
|
High
|
|
Internal Reflectivity |
Reduced and Heterogeneous |
Cystic spaces |
Absent |
High |
|
Height |
Variable |
Variable |
High |
Flattened |
|
In vivo confocal microscopy
|
Loose connective tissue |
Loose connective tissue and fluid-filled gaps |
Dense/fibrous connective tissue over large gap space |
Dense/fibrous connective tissue
|
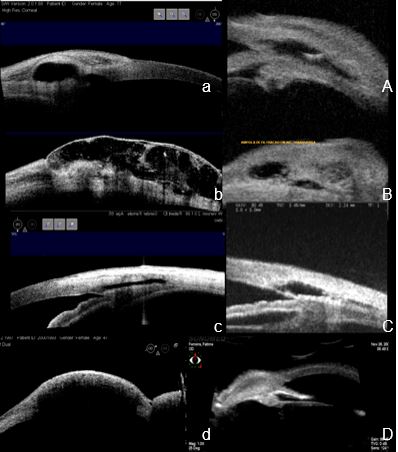
Figure 1. a and A a DIFFUSE filtering bleb: patent internal ostium, large intrascleral lake, low reflectivity and heterogeneous structure of the suprascleral tissue. b and B a POLICYSTIC filtering bleb: widespread low reflective suprascleral tissue with multiple coalescent low reflective spaces: c and C a FLATTENED filtering bleb: Trabeculo-Descemet’s window, intrascleral lake and route, high reflective suprascleral tissue: d and D an ENCAPSULATED filtering bleb: Suprascleral high reflective, tissue, large intrascleral lake. a, b, c, d AS-OCT; A, B C, D UBM.
The correlation between in vivo confocal microscopy findings and the AS-OCT filtering bleb reflectivity with the filtering glaucoma surgery outcomes has suggested that lower reflective and heterogeneous suprascleral tissue match with loose connective tissue, where gaps and high fluid content abound, thus documenting a functional bleb.5
UBM and AS-OCT can also assess several other glaucoma filtering surgery-related aspects, such as the:
• Patency of the glaucoma filtering surgery internal ostium (Fig. 2)
• Trabeculo-Descemet’s window integrity and thickness (Fig. 3 e 4);
• Intra and suprascleral lake dimension (Figs. 2,3,4);
• Presence of intrascleral route (Fig. 3);
• Fluid in suprachoroidal space (Fig.2);
• Reason for a non-functioning glaucoma surgery (Fig.5);
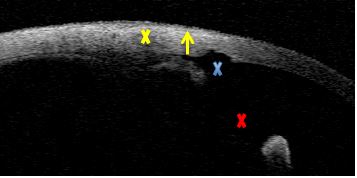
Figure 2. Trabeculectomy. Internal ostium patency (blue X), wide iridectomy (red X), suprascleral hyper-reflective tissue, scleral lake and route absent (yellow X), but subconjunctival low reflective line (yellow arrow). AS-OCT
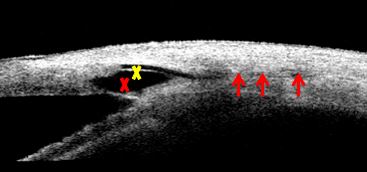
Figure 3. Non-penetrating deep sclerectomy. Intra scleral drainage implant (yellow X). Thin trabeculo-Descemet’s window. Wide sub scleral lake (red X) and posterior scleral route shown as a supra choroidal linear shadow (red arrows). AS-OCT
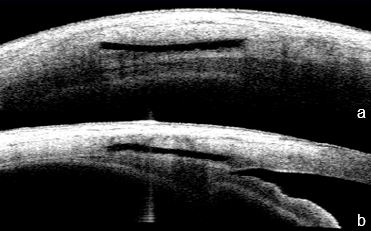
Figure 4. a. Non-penetrating deep sclerectomy. a. Horizontal section b. Radial section– polyedric scleral lake showing the non-reflective drainage implant, intact trabeculo-Descemet’s window, sub scleral route and heterogeneous reflective supra scleral tissue, suggesting a functioning bleb. AS-OCT
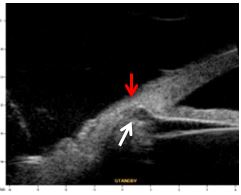
Figure 5. Non-functioning, non-penetrating deep sclerectomy. Iris (red arrow) and ciliary body (white arrow) hernia into the intrascleral lake, closing the angle and the trabeculo-Descemet’s window. UBM
Laser Iridotomy and Iridoplasty
The effect of laser treatment on ACA morphology can be followed up utilizing both UBM and the AS-OCT technologies. The high resolution cross section images they provide can clarify if a laser periphery iridotomy is completely permeable or not (Fig.3) and if the outcome of the former (Fig.3 An argon laser peripheral iridoplasty can be indicated before an acute attack of angle closure glaucoma, recurrent apposicional closure despite a patent iridotomy and the impossibility of creating a laser iridotomy because of hazy media. The effect of the procedure on the amplitude of the anterior chamber angle can be acknowledged by UBM or AS-OCT.6 (Fig.4 and Fig 5)
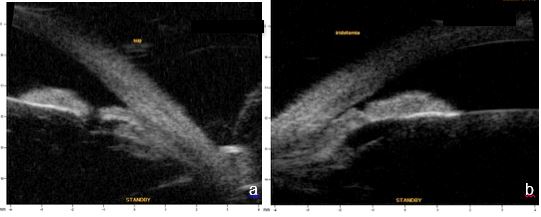
Figure 3a. Patent LPI, b. non-permeable LPI. UBM
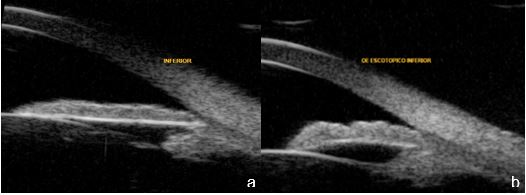
Figure 5a. Plateau iris before argon laser peripheral iridoplasty, b.Plateau iris after argon laser peripheral iridoplasty. UBM
Posterior Drainage Devices
UBM and AS-OCT can inform about the patency, route and relation of aqueous drainage devices with neighboring structures. Especially UBM can have a relevant role while planning this type of glaucoma surgery by allowing to assess the irido-ciliary sulcus and the anterior chamber angle to decide where to best place the proximal end of the valve tube. Fig.6
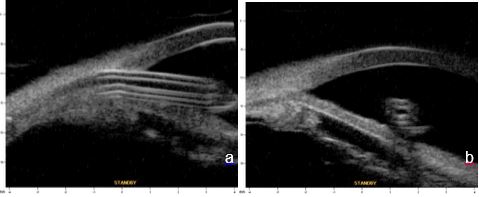
Figure 6 Posterior drainage device. a. Longitudinal tube section. b. Coronal tube section showing a patent lumen. Relation with the neighboring structures – proximity to the iris and distancing of corneal endothelium. UBM
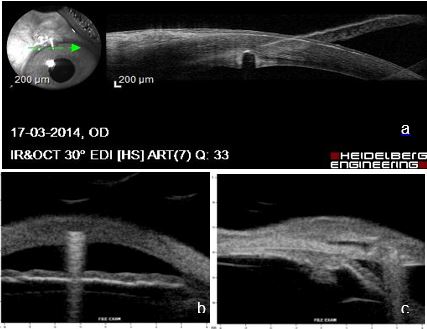
Figure 7 a. Gap in corneal tissue thickness suggesting anterior drainage device embedded in corneal tissue. AS-OCT. Due to its composition, this device shows by reverberation echoes. b. horizontal section – including cornea. c. radial section – anterior positioning of the device, and the intra-scleral lake and bleb ultrasound structure suggest active drainage. UBM
Minimal Invasive Glaucoma Surgery
The Minimal Invasive Glaucoma Surgery (MIGS) has been evolving associated to several devices such as the XEN Gel Stent® (AqueSys, Wisconsin Implant). This non-inflammatory soft, collagen-derived, permanent implant is injected ab interno to create an aqueous humor outflow path from the anterior chamber to the subconjunctival space.7,8,9,10,11 Figures 8 and 9 illustrate a case with good intraocular pressure control after the implantation of a XenGel Stent. 12
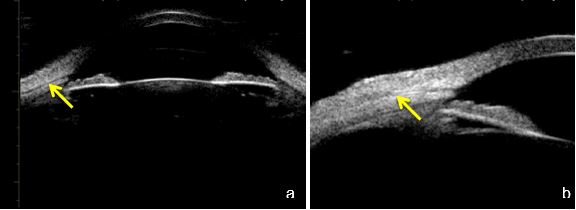
Fig. 8 a. Phakic eye (axial section) and b. (longitudinal section) showing a linear patent pathway (yellow arrow) through the sclera progressing towards the subconjunctival space. UBM
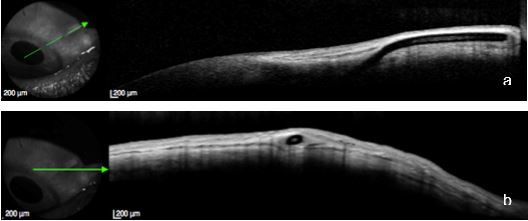
Fig 9. The same eye illustrated in Fig 23. a. Longitudinal and b. Cross-sectional views of the patent pathway and the diffuse filtering bleb generated by the device. AS-OCT
Viscocanalostomy
Very high frequency probes (80 MHz) enable the identification of Schlemm's canal, confirming it’s opening after viscocanaloplasty (Fig. 10).
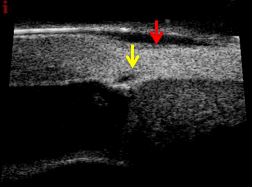
Figure 10 Schlemm's canal (yellow arrow) after viscocanaloplasty, Low reflective suprascleral tissue and suprascleral lake (red arrow). UBM (courtesy of Dr. Arabela Coelho)
AS-OCT technology allows presently better structural visualization of the Schwalbe’s line, trabecular meshwork and Schlemm’s canal than images acquired with the usual ultrasound probes of 35 and 50 MHz 13 (Fig. 11)
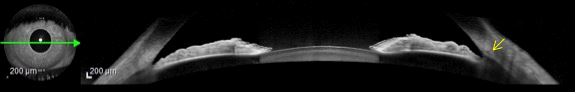
Figure 11. Schemm’s canal (yellow arrow) can be detected in AS-OCT imagiograms focusing the anterior chamber angle structures using Heidelberg technology. AS-OCT (Heidelberg Engeneering)
Cycloplastia
Ultrasound cycloplastia or high intensity focused ultrasound (HIFU) is currently being used to treat refractory glaucoma. Ultrasound waves are transmitted through a circular microdevice with six piezoelectric transducers that focus ultrasound emission on the ciliary body, promoting precise cycloplastia Evidence shows efficacy associated with intraocular pressure control, higher tolerance and safer profile when compared to other cyclodestructive techniques. Morphology alterations produced by circular ultrasound cyclocoagulation can be evaluated using UBM.14
UBM or AS-OCT allow the measurement of the anterior chamber width and select the best ring diameter to apply on the ciliary body and to check postoperatively the effects on the ciliary body. (Fig. 12)
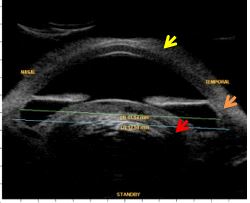
Figure 12 Measurements previous to ciliary high intensity focused ultrasound (HIFU). Corneal edema (yellow arrow), extensive peripheral anterior synechiae (orange arrow) and intumescent cataract (red arrow). UBM
Conclusion
AS-OCT and UBM technologies share overlapping features. Both provide high-resolution cross sectional images of the anterior segment structures allowing a detailed visualization of the anterior segment and anterior eye wall.
Both AS-OCT and UBM have shown to be useful in the post-operative assessment of glaucoma clarifying unexpected and unsuccessful outcomes and explaining the reason for the successful ones. AS-OCT provide very informative cross sectional images of the anterior segment anterior to da iris plane and of the eye wall, thus avoiding a contact examination to evaluate postoperative outcomes of filtering glaucoma surgery, of iris laser and surgery complications unrelated with the ciliary body.
Acknowledgements to
Dra. Manuela Carvalho, for her insurmountable encouragement and friendship
All Colleagues and Friends for having entrusted their Patients, whose corresponding images illustrate this paper.
